Designing healthcare apps isn’t just about making them functional – it’s about creating tools that are easy to use, accessible, and reliable for both patients and providers. Poor UX can lead to delays, errors, and frustration, while thoughtful design can improve outcomes and engagement. Here’s a quick summary of the 10 essential UX tips for healthcare apps:
- Simplify Navigation: Ensure clear, intuitive navigation for faster decision-making.
- Prioritize Speed: Optimize performance to avoid delays in critical scenarios.
- Go Mobile-First: Design for smaller screens first, then scale up for larger devices.
- Build Accessibility: Meet WCAG 2.2 AA standards to serve users with disabilities.
- Improve Onboarding: Use role-specific training and simple guidance for medical teams.
- Communicate Security Clearly: Use visible cues and plain language to show data protection.
- Add Offline Features: Enable access to critical data even without an internet connection.
- Encourage Medication Adherence: Use reminders, tracking, and subtle feedback to keep patients on track.
- Personalize with Smart UI: Tailor experiences based on user data and preferences.
- Enhance Provider Communication: Use secure, real-time messaging for seamless collaboration.
Quick Comparison Table
| UX Feature | Poor UX Example | Improved UX Example |
|---|---|---|
| Navigation | Confusing, multi-step processes | Intuitive, role-based workflows |
| Accessibility | Limited support for disabilities | Fully WCAG 2.2 AA compliant |
| Performance | Slow, frustrating load times | Fast, optimized for emergencies |
| Security Communication | Vague privacy policies | Clear, visible security cues |
| Offline Functionality | Rarely available | Works in low/no connectivity areas |
| Medication Adherence | Basic alarms | Personalized reminders and tracking |
| Personalization | One-size-fits-all design | Data-driven, user-specific features |
1. Create Simple Navigation for Clinical Workflows
Healthcare providers often make split-second decisions that can mean the difference between life and death. When they’re forced to sift through multiple screens to find patient information, it not only slows them down but increases the risk of errors, adds to their fatigue, and reduces overall efficiency.
A striking 94% of consumers emphasize the importance of easy navigation, and in healthcare, this becomes even more critical. Poorly designed navigation in medical apps can intensify cognitive overload, which is already high in clinical settings. As navigation expert Alan Cooper puts it, "Poorly designed navigation remains one of the most significant and common issues in interactive product usability". Healthcare apps need to do more than just function – they must seamlessly support workflows that are often life-critical.
Key Principles for Clinical Navigation Design
To create effective navigation for healthcare apps, simplicity and intuitiveness are essential. Here are some key principles:
- Clear pathways: Design straightforward routes for users, including clearly marked exit and return options.
- Thumb-friendly design: Place interactive elements within reach of the natural thumb zone for one-handed use.
- Hierarchical organization: Arrange information from general to specific, so users can quickly drill down to the data they need without feeling overwhelmed.
Familiar navigation patterns, like tab bars on iOS or navigation drawers on Android, are particularly useful in medical apps. These established designs help reduce the learning curve, especially during emergencies when medical teams need instant access to patient records, medication lists, or test results.
Real-World Success in Simplifying Navigation
A great example of improving navigation comes from Oscar Health. By reducing the number of navigational buttons in its app, the company made it easier for users to access essential features quickly.
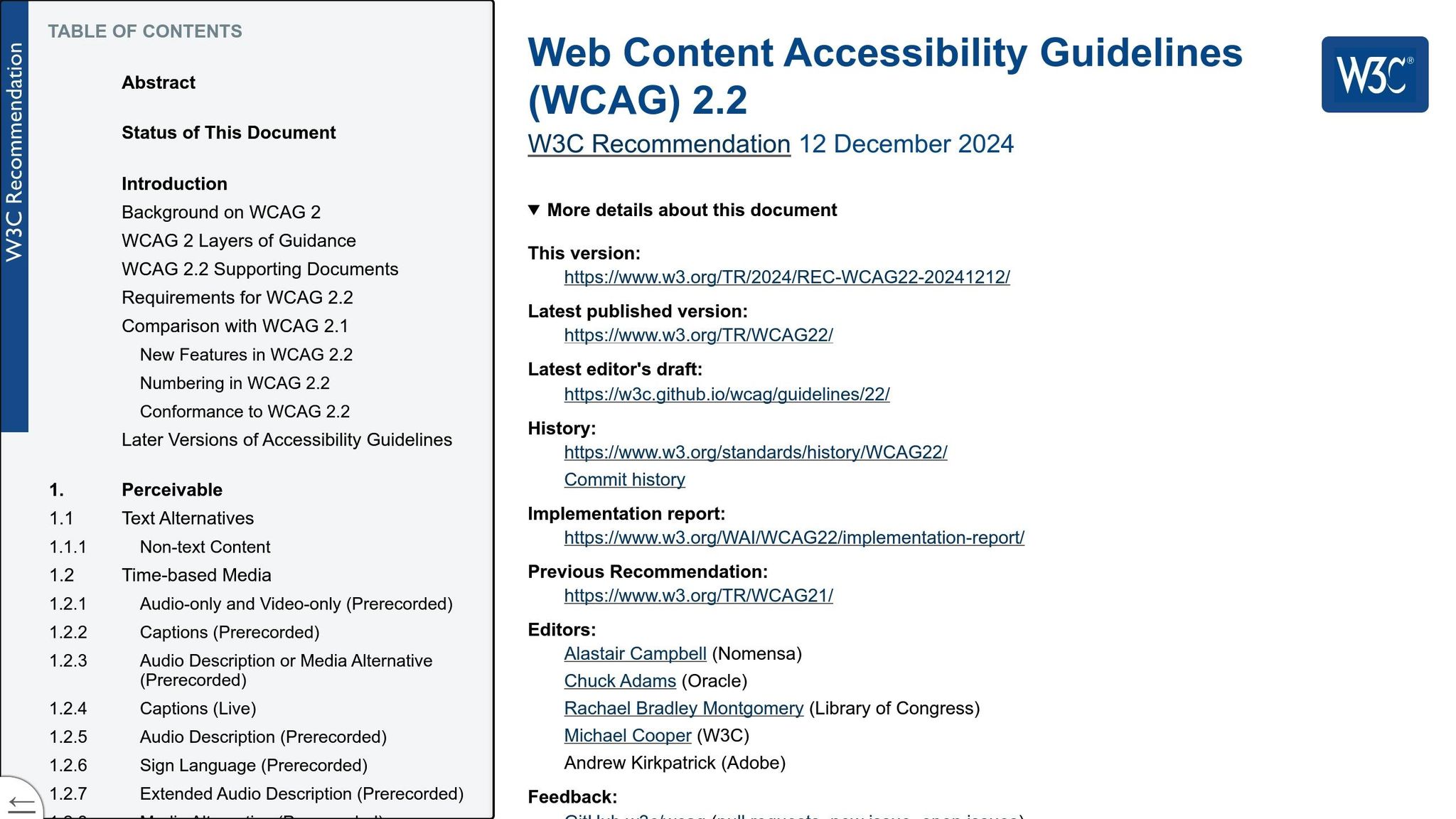
Accessibility and Compliance Standards
For healthcare apps, accessibility isn’t optional – it’s a necessity. Navigation design must comply with WCAG 2.2 AA standards, ensuring that users of all abilities can access critical healthcare information. This includes:
- Touch target sizes: Buttons and other touch elements must be at least 9 mm (about 0.35 in) to accommodate users with varying dexterity.
- Keyboard-only navigation: Apps should work seamlessly for users relying solely on keyboards.
- Color contrast: Maintain a minimum contrast ratio of 4.5:1 for normal text to ensure readability.
Screen reader compatibility is also vital, as roughly 2.2 billion people worldwide live with some form of visual impairment. Navigation elements must include proper ARIA labels and follow a logical tab order to align with assistive technologies.
Integration with EHR Systems
Healthcare apps don’t operate in a vacuum – they need to work hand-in-hand with existing Electronic Health Record (EHR) systems. Customizable interfaces tailored to specific medical workflows can greatly reduce cognitive load and speed up navigation. For example, allowing providers to configure dashboards, prioritize frequently accessed data, and create shortcuts for routine tasks can make a huge difference.
The most effective designs display relevant information together on a single screen. For instance, showing patient vitals, medication details, and recent test results side by side eliminates the need to jump between sections, enabling faster and better-informed decisions.
Platforms like MedMatch Network exemplify this approach. Their patient mobile app, MedmatchNet, integrates with existing EHR systems while maintaining intuitive navigation. This ensures that tasks like referral management, appointment scheduling, and accessing medical records follow consistent and familiar patterns across different healthcare touchpoints. With navigation simplified, the next priority should focus on optimizing app speed and performance for critical tasks.
2. Focus on Speed and Performance for Critical Tasks
In emergencies, every second matters. When healthcare providers need immediate access to critical patient data, even a small delay can have life-threatening consequences. Slow-loading apps not only frustrate users but can also lead to costly outcomes. In fact, 53% of users abandon a mobile site if it takes more than 3 seconds to load. In healthcare, where timing is everything, these delays can be catastrophic.
The stakes are even higher today, with telehealth usage soaring to 38 times pre-pandemic levels. This surge has placed immense pressure on mobile healthcare applications. When these systems falter, the impact goes beyond inconvenience – it can directly jeopardize patient care.
The Real Cost of Poor Performance
Healthcare organizations can’t afford to ignore performance issues. Poorly performing apps can cost organizations up to $2.49 million while also compromising patient outcomes. As Mav Turner from Tricentis points out, the healthcare sector often struggles to deliver reliable, high-quality mobile applications.
The data highlights the problem: 44% of users report buggy or slow app experiences, and 53% of users uninstall an app after just one crash or freeze. For healthcare providers, unreliable apps can mean abandoning essential tools at critical moments.
Strategies to Improve Performance
To ensure healthcare apps are fast and reliable, developers need to focus on efficiency at every level. This includes:
- Optimized Code: Streamlined algorithms, reduced redundancy, and efficient database queries are key, especially since healthcare apps handle large amounts of data like patient histories and medical images.
- Image and Media Compression: Using formats like WebP and implementing lazy loading ensures that visuals load quickly without straining the network.
- Content Delivery Networks (CDNs): CDNs distribute large amounts of data more effectively across regions, speeding up access to critical information.
- Caching: Storing frequently accessed data locally – such as vital signs, medication lists, and lab results – enables near-instant access, even under heavy server loads.
Lessons from Industry Leaders
Companies like Uber and Flipkart have set benchmarks for performance by leveraging custom networking libraries and Progressive Web App technologies. Healthcare apps can adopt similar strategies to deliver faster, more reliable experiences.
Handling High-Demand Scenarios
Healthcare apps must be prepared to handle peak usage without breaking down. Performance testing under high-demand conditions helps developers evaluate stability, response times, and server capacity. Real-time monitoring systems can also track performance and user behavior, allowing for quick adjustments as needs evolve.
The rollout of 5G technology promises to take healthcare apps to the next level. As Anastasia M., Tech Lead at TATEEDA, explains:
"5G enables real-time, high-volume data exchange for critical patient care."
Testing and Quality Assurance
Rigorous testing is non-negotiable. According to research, 81% of healthcare IT professionals consider usability, load, and security testing critical to ensuring app reliability. Automated testing is particularly promising, with 41% of senior IT professionals and developers believing it could cut organizational budgets by 51-75% annually.
Platforms like MedMatch Network exemplify these principles. Their MedmatchNet patient app integrates seamlessly with existing EHR systems while maintaining fast response times for critical features like referral management and appointment scheduling. By optimizing backend processes and utilizing advanced caching techniques, MedMatch Network ensures healthcare providers can access vital data instantly – even during periods of high demand.
Before focusing on cross-device compatibility, healthcare apps must first prioritize speed and reliability to meet the demands of critical care scenarios.
3. Use Mobile-First Design for On-Site Care
Mobile-first design has become a necessity in healthcare, with 87% of doctors and 85% of clinical educators relying on smartphones and tablets during patient care. By focusing on mobile-first strategies, healthcare providers can support faster, more effective clinical decision-making on-site.
The concept of mobile-first design begins with designing for smaller screens and then scaling up for larger devices. As the Interaction Design Foundation puts it:
"Mobile first design is an approach that embraces the constraints of smaller screens and focuses on what’s indispensable for users to improve the overall mobile User Experience (UX).”
This approach is especially important in healthcare, where 63% of healthcare searches now happen on mobile devices, and 53% of smartphone users check healthcare information over five times a day.
The Impact on Patient Care and Provider Efficiency
The benefits of mobile-first design go beyond convenience. For example, healthcare websites that aren’t mobile-friendly report 38% lower patient satisfaction rates. On the other hand, mobile-optimized sites boast conversion rates of over 20%, compared to just 3.6% for non-optimized ones.
Real-world examples illustrate these advantages. In May 2025, Alfred Health in South Melbourne reduced bounce rates by 27% after introducing thumb-friendly navigation zones tailored for larger hand spans. Similarly, Coviu, a telehealth provider, achieved a 33% reduction in bounce rates by implementing performance improvements like Brotli compression and deferred JavaScript loading.
Key Mobile-First Design Principles for Healthcare
Highlight Critical Information Immediately
Place essential features – like emergency contacts and booking options – at the top of the page. Use touch-friendly targets at least 48px in size and present critical health details in easy-to-read, scannable formats using progressive disclosure techniques.
Simplify Navigation for Clinical Needs
Navigation should be intuitive, even for one-handed use. Keep menus concise, with no more than five primary items. Use familiar icons and clear calls-to-action that remain functional in challenging environments, such as when providers are wearing gloves.
Ensure Readability for Medical Content
Medical accuracy depends on clear text. Use a font size of at least 16px with a line height of 1.5 for body text. Maintain high contrast ratios (minimum 4.5:1) to ensure readability, even in low-light conditions.
Performance Optimization for On-Site Care
In healthcare settings, network reliability can vary. To address this, use techniques like WebP image compression, lazy loading, and content delivery networks (CDNs) to ensure fast page load times.
A great example comes from Monash Health’s telehealth platform. By integrating WebRTC with TensorFlow Lite for offline symptom checking, they reduced failed consultations by 22% in May 2025.
Accessibility Matters
Mobile-first healthcare apps must accommodate users of all abilities. For instance, the Royal Children’s Hospital Melbourne achieved 100% WCAG compliance by using automated accessibility checks with Axe Core in their CI/CD pipeline. Including alt text for medical images and ARIA labels for interactive features ensures equitable access for all users.
Designing for Cross-Device Compatibility
Healthcare providers often switch between devices. Navigation should be thumb-friendly and responsive, adapting seamlessly across screen sizes from 320px (like an iPhone SE) to 1440px (desktop). This flexibility ensures smooth transitions between smartphones, tablets, and desktops throughout the workflow.
The MedMatch Network app shows how effective mobile-first design can be. By prioritizing referral management and appointment scheduling for mobile screens, the app ensures healthcare providers can access critical features anytime, on any device. Whether on a smartphone, tablet, or desktop, the interface stays consistent and reliable.
Mobile-first design aligns with the fast-paced realities of healthcare, ensuring that mobility and accessibility remain at the forefront of patient care. While this design approach solves many on-site challenges, the next step is improving communication between providers for seamless healthcare interactions.
4. Build Accessibility for All Patient Groups
Healthcare apps are designed to serve everyone, including the 1.3 billion people worldwide living with disabilities. These individuals often rely on healthcare services more frequently, making accessibility in app design absolutely critical.
In the U.S., about 1 in 4 adults has some form of disability. Yet, nearly 80% of the top hospital websites in the country fail to meet accessibility standards. That leaves millions of patients struggling to access essential healthcare information and services through mobile apps. This gap represents both a challenge and an opportunity for developers to create solutions that work for everyone.
Legal Requirements Push for Better Design
Regulations are stepping in to ensure accessibility is no longer an afterthought. In April 2024, the Department of Justice (DOJ) updated Title II of the ADA with the Web & Mobile Application Accessibility Rule, setting technical requirements for state and local government platforms. Shortly after, the Department of Health and Human Services (HHS) introduced regulations in May 2024, requiring healthcare apps to comply with WCAG 2.1 AA standards by May 11, 2026. These rules establish a clear framework for making apps accessible to patients with disabilities.
WCAG 2.2 AA: A Blueprint for Accessibility
Meeting WCAG 2.2 AA standards ensures healthcare apps are designed to be perceivable, operable, understandable, and robust for users with disabilities.
- Perceivable: Maintain a color contrast ratio of at least 4.5:1 for normal text and 3:1 for larger text. Allow users to adjust text size and include alternative text for images.
- Operable: Since nearly 80% of users with disabilities rely on screen readers, apps must be compatible with keyboard navigation. Simplify gestures to basic actions like tapping or swiping.
- Understandable: Use straightforward language to address the fact that up to 90% of Americans face challenges with health literacy. Keep layouts consistent to reduce confusion.
- Robust: Ensure the app works seamlessly with assistive technologies like voice recognition software and screen readers.
These principles create a strong foundation for developing apps that are accessible to all users.
Key Accessibility Features for Healthcare Apps
To make healthcare apps more inclusive, consider these essential features:
- Visual Accessibility: Offer adjustable text sizes for users with visual impairments and organize content with clear headings to improve navigation.
- Motor Accessibility: Design touch targets to be at least 9 mm in size with enough spacing around them, ensuring smooth interaction for users with limited motor skills.
- Auditory Accessibility: Add captions to all audio and video content to support users who are deaf, hard of hearing, or in noisy environments.
- Cognitive Accessibility: Simplify navigation paths and reduce visual clutter to lower cognitive load. Provide settings to customize font sizes, color schemes, and contrast levels.
A Smarter Development Approach
"People think quite often that building fully digitally accessible products and services means that it will add extra work. But that is not true. Because if you know how to do it, you can do it properly from the beginning." – Cezary Tomczyk, Former Apple accessibility expert
The secret to effective accessibility lies in designing with empathy. As Ahmed Khawaja, a Toptal Designer, explains, "We should be able to empathize with them so we can create a better solution". This means involving people with disabilities throughout the development process, integrating accessibility testing early, and using tools like semantic HTML markup and ARIA roles to improve functionality. When accessibility is baked in from the start, it benefits every user.
Beyond Compliance: Building Inclusive Experiences
Accessibility isn’t just about meeting legal requirements – it’s about creating apps that work for everyone. By 2030, 1 in 6 people will be over the age of 60, highlighting the growing need for features that address age-related changes in vision, hearing, and motor skills.
A great example is the MedMatch Network patient app, which was designed with accessibility in mind. It supports screen readers, allows keyboard navigation, and maintains high contrast ratios, ensuring it serves patients of all abilities effectively.
When healthcare apps prioritize accessibility, they improve the experience for everyone – whether it’s helping a patient use voice commands due to motor limitations or enabling a busy doctor to quickly find critical information. Starting with accessibility not only meets legal standards but also enhances the overall quality and usability of the app.
5. Improve Onboarding for Medical Teams
Onboarding in the medical field comes with its own set of challenges. Unlike other industries, healthcare professionals must quickly adapt to complex systems while continuing to provide uninterrupted patient care. With a projected shortage of 3.2 million healthcare workers by 2026 and data showing that active manager involvement makes employees 3.4 times more likely to view onboarding as successful, creating an efficient onboarding process is more important than ever.
Structured, role-specific training can ease this transition, reducing disruptions and administrative strain.
Start with Role-Specific Training Paths
Every role in healthcare comes with unique responsibilities, and training should reflect that. Tailoring onboarding to specific app features and workflows for each role ensures smoother transitions. For example, AbleTo, a mental health provider, expanded its network of clinical therapists and physicians from 200 to over 2,500 by implementing personalized in-app onboarding. Their approach included contextual training and continuous guidance.
"In two years, our provider community has grown 10x. It was vital to train this growing therapist community quickly and effectively, to meet demand, deliver top quality care, and improve outcomes. Whatfix’s contextual walkthroughs and smart tips personalize the learning process and provide 24/7 provider self-support – ensuring our providers are successful."
– Regina Owens, Director, Operations Learning and Development at AbleTo
Custom training plans that address both the clinical and workflow aspects of new systems are crucial for success.
Use Progressive Disclosure and Clear Objectives
Effective onboarding introduces functionality in manageable steps. Following the SMART framework – Specific, Measurable, Attainable, Relevant, and Timely objectives – helps medical teams grasp core features first, gradually moving on to advanced tools. For example, in an anesthesiology department, C8 Health‘s platform was rolled out with this approach, leading to 9 out of 10 users reporting daily time savings.
Design for Mobile-First Learning
Healthcare professionals often work on tight schedules, making mobile-friendly training essential. Apps should include bite-sized modules that can be completed during short breaks or between patient visits. Animated walkthroughs and visual demonstrations of tasks, such as medication administration or patient data entry, can simplify complex workflows and speed up learning.
Build Trust Through Transparency
Medical professionals are naturally cautious about adopting new technology, especially when it impacts patient care. Onboarding should emphasize the app’s core features, benefits, and data security measures. Providing clear navigation tools – like a "back" button or a visual progress tracker – and allowing users to skip non-essential sections can build trust by respecting their time. A transparent, role-focused onboarding process sets the stage for long-term user confidence and satisfaction.
Provide Ongoing Support and Feedback Loops
Onboarding doesn’t stop once initial training is complete. Regular check-ins and feedback collection are essential for refinement. One example is a national Medicaid health plan that developed standardized workflows for provider onboarding. By incorporating automation, they reduced turnaround times, improved data accuracy, and secured stakeholder buy-in within three months.
Similarly, MedMatch Network offers role-specific tutorials and contextual guidance for physicians, specialists, and administrative staff. This targeted approach significantly reduces the learning curve for busy medical teams.
When healthcare apps prioritize empathetic, role-specific onboarding, they shift from being potential workflow hurdles to becoming indispensable tools that enhance patient care and streamline administrative tasks. This thoughtful approach ensures both immediate and long-term success.
6. Communicate Security Through UX Design
Healthcare apps handle some of the most sensitive personal data imaginable, so it’s crucial to make security visible and understandable through design. When users can’t see or grasp how their medical data is safeguarded, trust erodes quickly. Instead of burying security details in lengthy, hard-to-read privacy policies, visual design should clearly highlight the protective measures in place.
The key challenge is to present these security measures in a way that’s obvious and reassuring to users. Both healthcare professionals and patients need visual confirmation that their private information is secure at every stage of interaction. This is where visible security cues can play a pivotal role in reinforcing trust.
Make Security Features Visible and Accessible
Strong authentication measures should feel natural and easy to use, not like a hassle. Features such as multi-factor authentication and biometric security should come with clear visual indicators that guide users through the process and explain how these steps protect their data. For instance, when users encounter a fingerprint icon or face recognition prompt, a short explanation like “This step ensures your medical records remain private” can provide clarity and reassurance.
Context is everything when it comes to visual security cues. Icons like locks, encryption badges, or security indicators should appear exactly where users interact with sensitive information. For example, a green checkmark next to a message like “Data encrypted” during file uploads can deliver instant peace of mind without interrupting the user’s workflow.
Design Transparent Privacy Communication
Privacy policies filled with legal jargon can confuse users and undermine trust. Instead, healthcare apps should strive to explain data collection and protection in plain, straightforward language. Key security details should be integrated directly into the interface, making them easy to find and understand.
A great example of this is Onix’s platform for British cancer patients. They incorporated simple, granular privacy controls, allowing users to decide who could access their information – whether it was everyone, just friends, or no one but themselves. This approach made privacy settings intuitive and gave users a sense of control over their data.
Build Trust Through Progressive Security Disclosure
When it comes to sharing security information, less is often more – at least initially. Start with the essentials, such as a message like “Your data is HIPAA-compliant and encrypted,” and offer more technical details through a “Learn more” link for those who want to dive deeper.
Displaying trust badges and certifications prominently can also strengthen credibility. HIPAA compliance badges, third-party certifications, and security audit results are powerful visual tools that help users quickly assess the app’s reliability without cluttering the design.
Implement Secure Messaging with Clear Visual Indicators
Communication within healthcare apps demands special attention to security. Encrypted messaging should come with unmistakable visual indicators, such as a shield icon or an “Encrypted” label, to confirm that conversations are protected.
For example, MedMatch Network ensures secure communication by clearly showing when data is encrypted. This seamless integration of security cues into the platform’s interface reinforces user confidence while maintaining a smooth user experience.
sbb-itb-c710a24
7. Add Offline Features for Emergency Use
Healthcare apps need to function reliably even without an internet connection. In emergencies or low-coverage areas, uninterrupted access to patient data can be a lifesaver, enabling healthcare providers to make informed decisions without delays. Building offline functionality into these apps ensures critical information is always available, no matter the connectivity status.
This is especially crucial in settings like emergency rooms, rural clinics, and mobile care units, where network issues are common. By storing essential data locally on devices and syncing it back to servers when the connection is restored, apps can help maintain seamless patient care.
Design for Critical Data Access
Focus on offline access to key information like patient histories, medications, allergies, and treatment plans. With 70% of users expecting apps to work offline, it’s essential to store frequently used data locally. Adding clear visual indicators to show when the app is in offline mode can help users navigate confidently during connectivity issues.
Implement Smart Data Synchronization
A robust synchronization system is vital to merge offline updates with the central Electronic Health Record (EHR) once a connection is reestablished. It should also handle conflicts when multiple users update the same patient record offline. This approach ensures the app remains reliable and up-to-date.
Take the Simple app as an example. Used across 400 hospitals to manage care for 190,000 hypertension patients, it allows nurses to input data even in low-connectivity areas. Every second saved during patient interactions adds up to significant efficiency gains. Govind Joshi from Simple highlights this advantage:
"Going offline-first was one of the best decisions we made in our technical architecture… We have seen clinicians treating up to 200 patients in a single day – every extra second in a patient interaction at that velocity multiplies quickly."
Optimize Performance and Storage
Offline functionality must balance performance with device limitations. Managing how often data is pushed or pulled can conserve battery life and storage. Prioritize storing only the most critical data locally and use tools like UUIDs (Universally Unique Identifiers) to prevent conflicts during synchronization. This ensures the latest updates are accurately reflected across devices.
Communicate Offline Status Clearly
Make it easy for users to understand the app’s connectivity status. Use clear visual cues to indicate when the app is offline and provide quick access to cached data. Progressive Web Apps (PWAs), which store data locally, not only load faster but also see 50% higher engagement compared to native apps.
8. Use Small Interactions to Improve Medication Adherence
Small, thoughtful interactions within healthcare apps can make a big difference in keeping patients on track with their medications. Features like reminders and progress tracking create consistent touchpoints that reinforce treatment routines. This is critical when you consider that missed doses or incomplete treatments contribute to 125,000 preventable deaths annually and cost the U.S. healthcare system over $300 billion.
One simple yet powerful tool is personalized reminders. When apps tailor notifications to fit a patient’s specific schedule, adherence rates can improve by 13%.
Design Reminders That Actually Work
A good medication reminder is more than just a basic alarm. Leading healthcare apps allow users to customize reminders for each medication, taking into account dosing schedules, meal timings, and individual preferences. Visual aids like pill images, color-coded charts, and clear dosage labels make it easier for patients to identify their medications. Accessibility features such as voice alarms, large fonts, and user-friendly navigation ensure these tools work for everyone, including those with disabilities or vision challenges. With 46% of Americans using prescription drugs monthly, these thoughtful designs address both simple and complex medication routines.
Track Progress to Build Momentum
Tracking tools turn medication adherence into a measurable and motivating journey. Apps that allow patients to log their medication intake and monitor their progress over time help build consistency and confidence. In fact, healthcare apps with strong user experience can boost adherence by 40%. A great example is the MySugr app, which supports diabetes management by tracking blood sugar levels, sending medication reminders, and sharing data with healthcare providers. Its intuitive design has resulted in a 72% increase in user engagement compared to less user-friendly apps.
Use Subtle Animations and Feedback
Small design touches like animations and instant feedback can make a big impact. For instance, when a patient marks a medication as taken, a quick animation or color change provides immediate confirmation. These microinteractions reduce uncertainty and create a sense of accomplishment. Adding gamification elements, like achievement badges for staying on track, can further motivate users. However, it’s important to keep these animations subtle to avoid overwhelming the user.
Integrate Educational Resources
Educational tools within apps can also improve adherence by helping patients understand the importance of their medications. Smart app designs prioritize critical information while keeping secondary details hidden until needed, avoiding information overload. Chatbots offering real-time answers to common questions can ease concerns and build confidence. Features like auto-save and AI-assisted predictive text simplify the process of logging daily medication, making it less of a chore.
The benefits of these small interactions go beyond individual patients. Engaged users experience 14% fewer hospital readmissions, showing how well-designed healthcare apps can positively impact the broader healthcare system. By focusing on these details, apps can foster lasting patient engagement and better health outcomes.
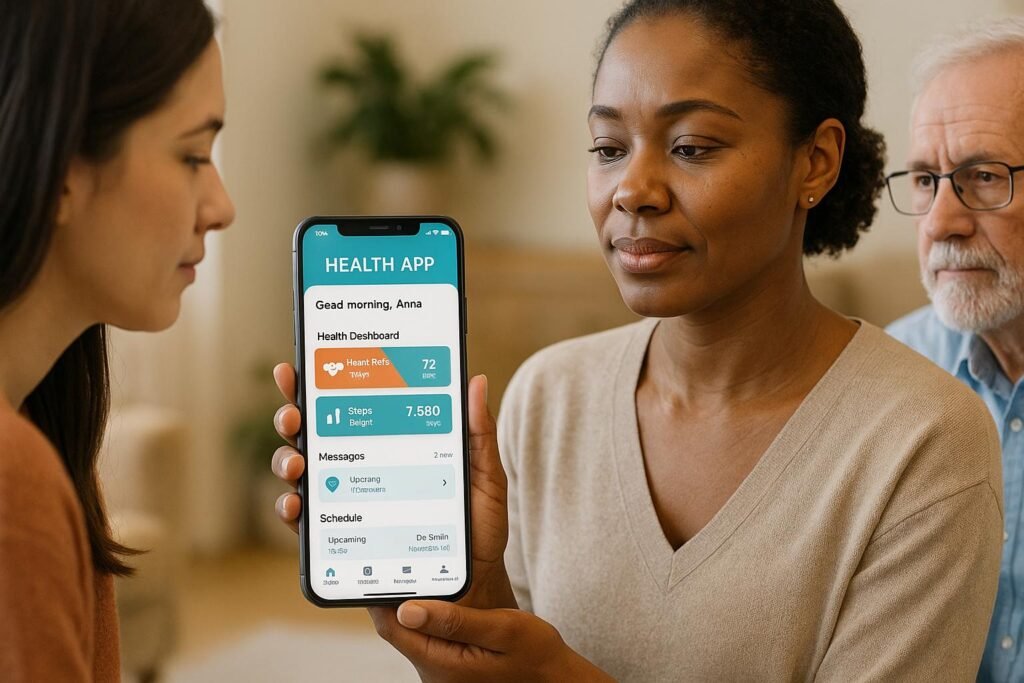
9. Customize Patient Experiences with Smart UI
Smart UI takes healthcare apps from being one-size-fits-all tools to personalized platforms that cater to each patient’s specific needs. By analyzing individual data and preferences, these interfaces not only enhance satisfaction but also improve health outcomes. With 63.4% of U.S. adults using health-related apps in the past year and digital health revenue projected to hit $193.69 billion in 2024, it’s clear that the demand for tailored healthcare solutions is skyrocketing.
The strength of smart UI lies in its ability to seamlessly process multiple data streams. Apps can now adapt to patients by factoring in socio-demographics, health records, personal preferences, digital literacy, and even environmental sensor data. This creates a highly responsive system that delivers what patients need, exactly when they need it. Such capabilities set the stage for advanced, data-driven personalization.
Data-Driven Personalization That Delivers Results
Modern apps leverage AI to study user behavior and predict what content will be most relevant. For healthcare organizations, this approach has delivered tangible benefits. Personalization has led to a 10% increase in customer satisfaction, reduced administrative expenses by up to 10%, and improved quality standards by 20–25% within just 6–12 months. These numbers highlight how smart UI is quickly becoming a cornerstone of effective healthcare services.
Personalized Content for Individual Health Needs
Smart UI enables apps to deliver content and messages tailored to each patient’s health journey. Instead of offering generic advice, patients receive updates and tools specific to their medical history and current conditions. For example, a diabetes patient might get blood sugar tracking reminders and meal-planning tools, while a cardiac patient could see features for exercise tracking and medication schedules.
Real-time data integration takes this one step further. Apps can adjust dynamically based on a patient’s behavior or health status. If a patient misses medication or their activity level drops, the app can respond with motivational messages or additional support tools. This level of personalization ensures patients stay engaged and supported at every stage of their care.
Unified Patient Profiles for Seamless Experiences
Unified patient profiles bring data from EHRs, wearables, and app interactions together, ensuring consistent personalization across all platforms. Whether a patient is using a mobile app, visiting a website, or receiving email updates, the experience feels cohesive and tailored to their needs.
Platforms like MedMatch Network exemplify this approach by integrating referral data, appointment histories, and provider communications. This ensures a smooth, personalized experience that spans the entire care process.
Customizable Interfaces for Maximum Comfort
Smart UI doesn’t stop at content – it also extends to the app’s layout and usability. Patients can tweak their interface by selecting favorite features, organizing widgets, or enabling options like dark mode. Even small touches, such as optimizing for left- or right-handed users, make the app more comfortable and accessible.
Through real-time analytics and predictive suggestions, apps can anticipate what users might need next. This level of customization is crucial, especially when 70% of healthcare consumers say they’d switch providers for a more tech-friendly experience.
Ultimately, smart UI represents a shift toward technology that adapts to people, not the other way around. By creating personalized, intuitive experiences, healthcare apps can not only boost patient satisfaction but also drive better health outcomes across a wide range of patients.
10. Support Provider Communication Through Smart Messaging
Smart messaging has become a game-changer for provider communication, a cornerstone of effective patient care. Traditional methods often lead to delays or misunderstandings, which can jeopardize outcomes. In contrast, smart messaging ensures secure, real-time communication, keeping care teams connected no matter where they are.
A study conducted at Washington University and BJH Healthcare revealed some striking numbers: over six months, daily message volume increased by 29%, with nearly 33,000 users exchanging over 9.6 million messages across 74 different healthcare roles. The median message length? Just 41 characters. This brevity highlights how healthcare professionals can share critical updates quickly and efficiently, ensuring communication stays on point as teams coordinate care.
Real-Time Collaboration Across Disciplines
Smart messaging eliminates the barriers between healthcare specialties, fostering collaboration. For example, inpatient messages are most frequently exchanged between nurses and physicians (20%), followed by physicians to nurses (13%). In outpatient settings, 16% of messages flow from physicians to nurses, while 11% occur between medical assistants. This type of cross-functional communication allows teams to share insights, discuss treatment plans, and make timely, informed decisions.
Security and Compliance at the Core
In healthcare, messaging isn’t just about speed – it must also adhere to strict regulatory standards. HIPAA-compliant messaging platforms make it easy for care teams to send instant messages, share files, and even hold voice or video calls while safeguarding sensitive health information.
"HIPAA compliant instant messaging is a secure method of communication that requires minimal set up, configuration, and instruction, as most of the required safeguards are installed by default on mobile and desktop apps." – Steve Alder, Editor-in-Chief, The HIPAA Journal
Key security features include end-to-end encryption, stringent access controls, and audit trails that monitor user activity to ensure compliance.
Features That Improve Care Coordination
Modern messaging platforms go beyond simple text exchanges, offering advanced tools like priority notifications, message delegation, and group chats. Priority notifications ensure urgent messages grab attention until they’re addressed. Message delegation allows team members to reassign tasks when they’re unavailable. With around 70% of the global population owning smartphones, these features are vital for maintaining seamless communication in healthcare settings.
These tools not only enhance clinical collaboration but also simplify administrative processes, making it easier for teams to stay organized and responsive.
Simplifying Administrative Tasks
Smart messaging isn’t just for clinical updates – it also streamlines administrative work. From scheduling to sending announcements, secure messaging enables providers to consult specialists, share test results, and seek advice quickly, especially in emergencies.
Platforms like MedMatch Network take this a step further by integrating secure messaging with referral management and EHR systems. This integration removes the hassle of switching between platforms while maintaining compliance and security standards.
"Analyses of patterns and content of secure messages could help facilitate at-scale identification of areas for improved team functioning, delivery of clinical care, and design of EHR tools." – Physicians from the University of Michigan and the University of California, San Francisco
It’s clear that smart messaging is no longer just a convenience – it’s becoming a critical part of modern healthcare infrastructure. By adopting secure, feature-rich messaging systems, healthcare organizations can boost communication efficiency, improve patient safety, and foster a more collaborative care environment.
Comparison Table
Standard UX vs. Improved UX in Healthcare Apps
Here’s a breakdown of how standard UX differs from improved UX in healthcare apps, focusing on critical elements like navigation, accessibility, and performance:
| Feature | Standard UX Approach | Improved UX Approach |
|---|---|---|
| Navigation | Complicated, multi-step processes that confuse users | Simplified workflows with role-based dashboards |
| Accessibility | Limited adherence to accessibility standards | Fully aligned with WCAG 2.2 AA guidelines |
| Performance | Sluggish loading times that frustrate users | Optimized for speed and reliability |
| Security Communication | Minimal or unclear security messaging | Transparent, user-friendly security explanations |
| Offline Functionality | Rarely available when needed most | Designed with emergency scenarios in mind |
| Information Architecture | Overwhelming data presented all at once | Progressive disclosure with key data prioritized |
| User Testing | Little to no accessibility testing | Frequent testing with users who have disabilities |
This comparison highlights how improved UX tackles the shortcomings of standard designs, leading to better patient engagement. Enhanced UX doesn’t just make apps easier to use; it boosts patient satisfaction, reduces drop-off rates, and even improves clinical outcomes. Considering that about 1 in 4 adults in the U.S. live with a disability, and 2.2 billion people globally experience some form of visual impairment, accessible design isn’t just a feature – it’s a necessity.
Take MyChart, for example. Its intuitive interface lets users manage appointments, view test results, and communicate with healthcare providers effortlessly. It also integrates with fitness trackers, enabling seamless data sharing with doctors. Similarly, Babylon Health leverages AI-driven UX to analyze data like activity levels and heart rate, offering personalized medical advice through an easy-to-navigate interface.
Standard UX often frustrates users with clunky consent screens and vague privacy notices, which fail to enhance security. Improved UX, on the other hand, integrates regulatory requirements smoothly. Features like multi-factor authentication and biometric security protect user data without sacrificing usability.
The impact of investing in better UX design is clear. Research published in the Journal of Medical Internet Research shows that well-designed healthcare apps and websites can increase patient satisfaction by up to 60%. With over 375 million mobile health app downloads in 2023 and a growing population of older adults – 1 in 6 people will be over 60 by 2030 – modern healthcare apps must adopt these improved UX principles. Poor usability already leads 30% of patients to abandon telehealth platforms, making the shift to better UX critical for patient retention and engagement.
Conclusion
Creating outstanding UX for healthcare mobile apps goes far beyond following design trends – it’s about making a real difference in patient care and clinical efficiency. The ten tips shared in this article lay the groundwork for developing apps that genuinely benefit both patients and healthcare providers.
This focus on user-centered design isn’t just a nice idea; it’s backed by measurable results. For instance, a 2015 study in the Journal of Informatics in Health and Biomedical revealed that only 36% of top EHR vendors showed strong user-centered design practices, even though physicians spend over six hours daily using EHR systems. Clearly, better design can address significant challenges in healthcare technology.
Applying these UX principles can lead to higher patient engagement, reduced administrative workload, and improved clinical outcomes. Features like large, easy-to-use controls, intuitive navigation, and automatic data visualization allow healthcare professionals to concentrate on what truly matters – caring for their patients.
Real-world examples highlight how smart UX design can transform healthcare. Take MedMatch Network, for instance: by applying user-focused design principles, the platform cut neurology referral times from 30 days to just 18 – a 40% reduction. It also sped up preoperative evaluations by 25% and boosted patient engagement by 50%.
With the global mHealth market expected to hit $115.61 billion by 2025, the demand for apps that go beyond basic functionality to offer patient-centered experiences is only growing. To meet this demand, developers must prioritize user research, iterate designs based on feedback, and ensure every feature is simple and accessible.
Designing for healthcare isn’t just about aesthetics – it’s about balancing compliance, clinical accuracy, and usability. Apps that combine intuitive navigation, accessibility for all users, and visible security features not only improve workflows but also empower both providers and patients. The best apps make these elements feel seamless, delivering secure, functional, and user-friendly experiences.
Ultimately, the future of healthcare lies in technology that prioritizes the user. Every design choice – from how navigation works to how security is communicated – directly impacts how well providers deliver care and how effectively patients manage their health. Investing in thoughtful UX isn’t just about better apps; it’s about better health outcomes for everyone.
FAQs
How can healthcare mobile apps balance accessibility and a smooth user experience?
Healthcare apps can strike a balance between being accessible and delivering a smooth user experience by adhering to the Web Content Accessibility Guidelines (WCAG) and embracing inclusive design principles. Features like adjustable text sizes, high-contrast color schemes, and compatibility with screen readers not only make the app functional for individuals with disabilities but also enhance usability for everyone.
To comply with regulations such as the Americans with Disabilities Act (ADA) and ensure continued usability, it’s important to conduct regular accessibility audits. These audits help pinpoint and address potential barriers, making the app easier to use for people with disabilities, temporary impairments, or those in less-than-ideal conditions. Prioritizing accessibility allows healthcare apps to create a more user-friendly and welcoming experience for all.
How can healthcare apps ensure fast and reliable performance during periods of high demand?
To keep healthcare apps running smoothly during busy times, it’s crucial to prioritize scalability. Using a cloud-based infrastructure allows apps to automatically adjust resources to meet spikes in traffic, ensuring they perform reliably even at peak usage.
On top of that, performing regular stress tests can help pinpoint weak spots that might struggle under heavy loads. Combine this with real-time monitoring to catch and fix performance issues as they happen, guaranteeing users a seamless experience when it matters most.
Why are offline features important for healthcare apps, and how can they be effectively implemented?
Offline features play a crucial role in healthcare apps, ensuring users can access vital information even when internet connectivity is poor or completely unavailable. This becomes especially critical during emergencies or in remote areas where reliable internet access is not an option. By offering offline functionality, healthcare apps can maintain patient engagement and allow providers to deliver uninterrupted care.
To make offline features work seamlessly, focus on providing access to essential functions like viewing medical records, logging health data, or checking appointment details. This can be achieved by using local storage methods, such as caching or device-based databases, to temporarily save data. Once the app regains an internet connection, it can automatically sync the locally stored data with the server. This approach not only ensures data accuracy but also delivers a smooth user experience, reducing the stress of connectivity issues.