Why I Founded MedMatch
MedMatch Network: Founder’s Story
by Dr. Amos O. Daré, MD, FACS, Founder & CEO of MedMatch

Introduction
Like most of my colleagues, I chose to become a physician and a surgeon to save lives. The rude awakening that awaited me after medical school was realizing that we do not practice medicine in a void. Of course, there are plenty of patients needing help. However, I quickly realized that on this side of the Atlantic, where the level of medical care stands at one of the highest in the world, the patient’s ability to pay for their care is a constant constraint on effective healthcare delivery.
In the US, the purse-strings of medical care rest in the hands of managed healthcare organizations. With the advent of the Health Maintenance Organizations (HMOs), Point of Service (POS), and Preferred Provider Organizations (PPOs) in the 1980s, a physician must either be contacted by a patient’s health insurance organization or be a “preferred provider,” to be appropriately compensated.

Therefore, in our current healthcare reimbursement system for providers, unless the patient is paying out-of-pocket for the entire medical service, a patient is required to be matched to a physician that participates in his/her healthcare insurance network. For example, I may know another physician who I believe is best qualified to help manage my patient, but unless I am in an emergency or hospital environment, I will need to research and determine if the physician is in the patient’s health insurance network. The requirement to match a patient to a physician who takes their insurance has effectively created a front office task for the physician. This is not a small task. It is the cause of frustration and anxiety for many physicians and their patients, and something that I have personally experienced.
Lack of patient information.
A patient came to see me with a recent diagnosis of a brain tumor. I determined that the patient will likely need surgery to address her condition. In assessing her candidacy for the procedure, I needed to confirm her overall health condition was strong enough to undergo anesthesia and the surgery itself, in addition to investigating chest pains she had noted. Therefore, I not only needed to refer her to a primary care physician, but also a cardiologist.
The last thing we wanted was the surgery to be her stress test! If her heart were not strong, she would not survive the surgery.
The Referral Process
We can break down the referral task explained above into five steps.

The first step is to identify a physician that takes the patient’s insurance, broken down to: first finding the physician, then making sure that the physician accepts the patient’s insurance. Finding a physician could be done simply from memory recall, past referrals, recent encounters, or the age-old word-of-mouth method. If all fails, there are several “Find a Doctor” resources available online. Verifying if the physician takes the patient’s insurance can be accomplished by checking information on the physician’s website, the insurance company’s website, or by placing a phone call to the physician’s office.

After identifying the physician and confirming he/she is within the patient’s insurance network, the second step is to schedule the patient. To schedule the appointment, my staff will often use phone, fax, email, and in some instances, fill out forms on a provider’s website to transmit the referral request.

The third part of the referral process deals with insurance pre-authorization. Without prior approval for the visit by the health insurance organization, the receiving physician would likely not be compensated by the patient’s insurance. Therefore, in many instances, the PCP is burdened with getting insurance authorization for the specialty consultation, receiving constant reminders from the specialist office.

There need to be successful continuity or transfer of care from the referring physician to the receiving physician. Either the referring physician will take on the responsibility to call and inform the patient of their appointment once a time has been secured, or the receiving physician will reach out to the patient to schedule/ confirm the appointment and complete a checklist before the visit.

The referral is not complete until the referring physician receives the consultation note. The referral was originated to solicit the opinion of a specialist or a colleague and help manage the patient. The referring physician cannot complete their management or develop a plan of care for the patient until they receive the consultation report.

The Challenges
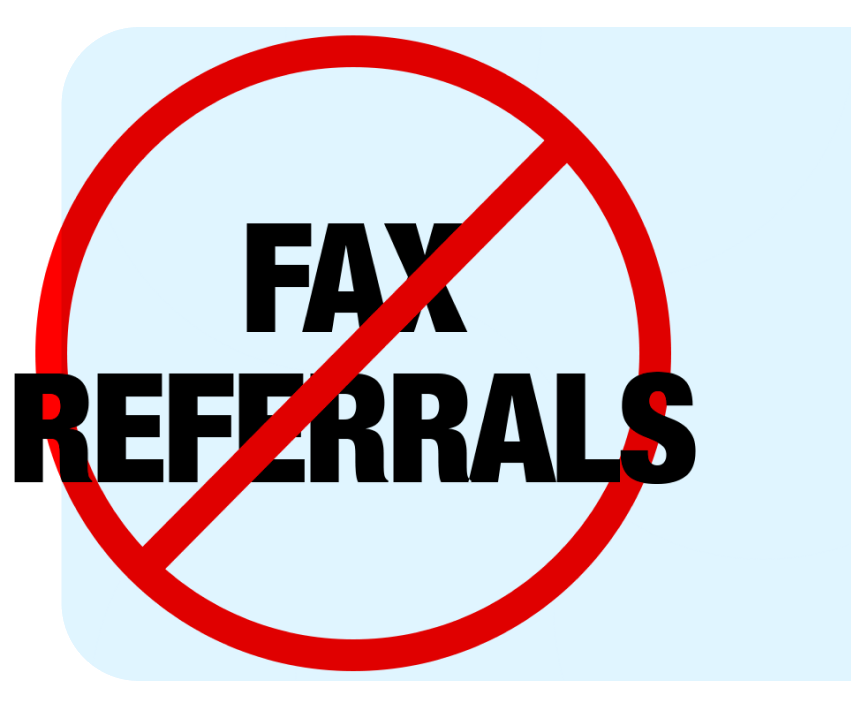
The current referral protocols and software used in many medical offices today are archaic, rely significantly on staff, and are poorly automated. Some current office electronic health record (EHR) systems may initiate the referral by either fax or email but have no ability to track and ensure that the referral is completed. These are unsophisticated systems, and much can go wrong at each of the steps outlined above.
Step one
Can be time-consuming, especially without readily accessible, up-to-date physician databases that prequalify physicians for a particular referral in some geographic regions. Frequently, my staff is waiting on the phone for several minutes. There may be a need to call several times and/or leave messages that never get returned. Should the initial transfer of information be unsuccessful, there is often no way to know. It can take several days to find a readily available physician that accepts the patient’s insurance.

In step two
It is not uncommon for my staff to call a physician that they have identified in step one, only to be told that the physician is not accepting new patients. In this case, we are back to square one! In other cases, receiving physicians may not acknowledge the initial referral. They will try to reach out to the patient to schedule the appointment and if the office is unsuccessful, there is no connection to the referring physician to confirm the referral. This can be labor-intensive for the front office, and sometimes for the patient. Patients who get involved in their referral are often frustrated by the process.
Generally, it is the culture of the medical office to give priority to calls from other medical offices or professionals. Offices will often have multiple incoming phone lines to separate calls from patients and healthcare providers, with the latter given a higher priority. I have heard of patients reporting, “It’s been four weeks since my doctor put in a geneticist referral for me, and they haven’t even called to schedule.”

In the third step
I have had patients show up in my office with insurance authorization still pending for appointments that were scheduled days or even weeks ahead. Further, the confusion is not always because the insurance company did not approve the visit. Instead, it may simply be due to a lack of coordination or appropriate reminders for the doctor’s office to submit all the forms required for approval.
Fourth Step
Responsibility for the fourth task of communicating the referral and appointment falls in the gray area between the referring and receiving physicians and the patient. Unfortunately, it is during this handover that the referral “baton” can be dropped. This step could be sabotaged simply by not reaching the patient with reminders, appointment time, and confirmations.

Fifth Step
Due to the simple fact that most referring physicians have no way to track their referrals, step five is at risk of falling through the cracks. As in step two, where the receiving physician may never acknowledge the referral in the first place, in this step the referring physician may not know if the patient was seen unless they received a report from the specialist. In a recent survey, up to 50% of primary care physicians did not know if their patients were seen by the specialist. In most instances, it is up to the patient to “sound the referral alarm.”

We can do better!
As a society, we can certainly do better. As a physician and technology enthusiast, I am compelled to advocate for technology in medical referral management and I am privileged to participate in its implementation.

— Amos Dare MD, FACS
Founder and CEO

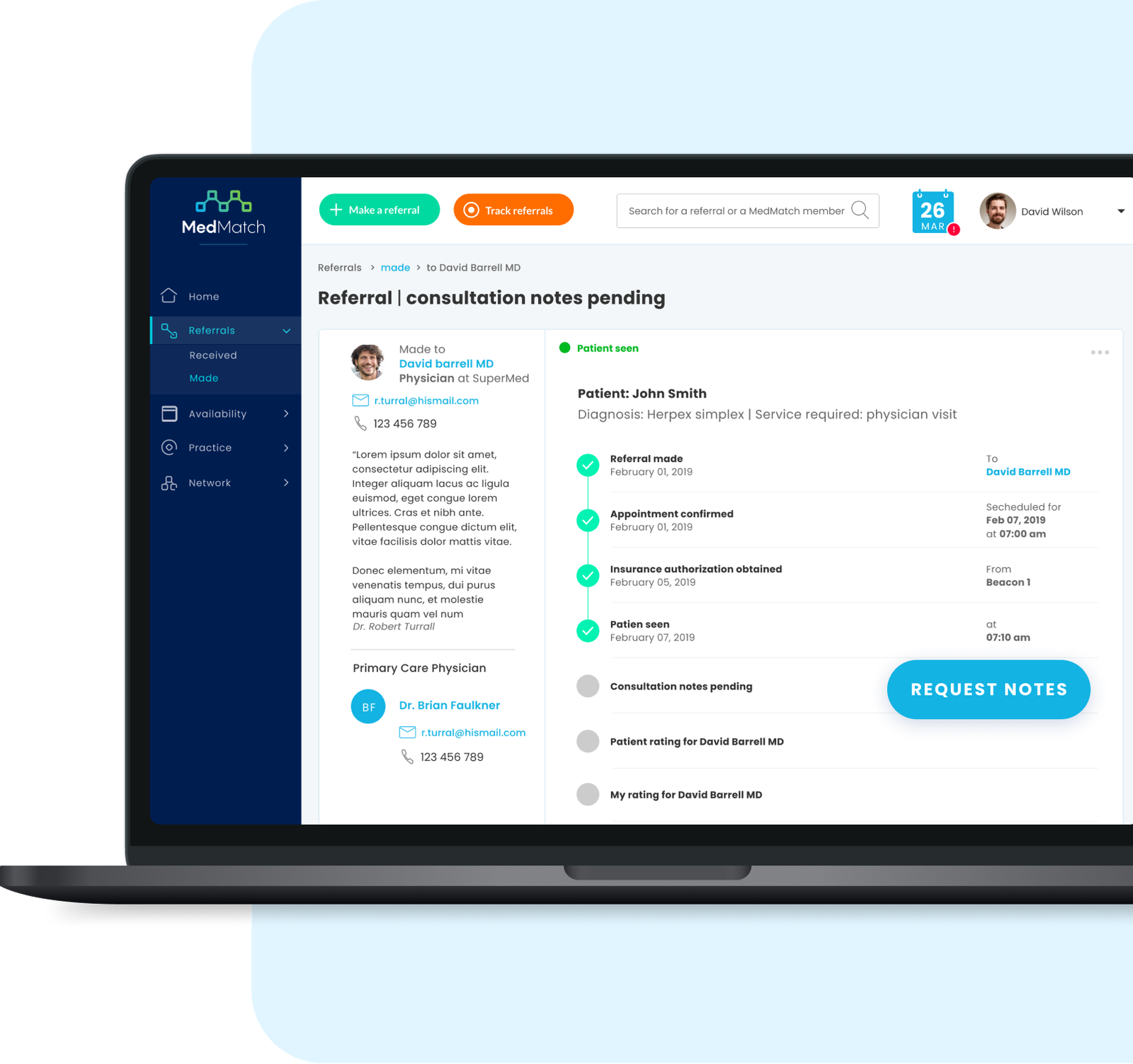
While the priority is consistently delivering optimal patient care, the referral process is often taken out of a doctor’s hands. Our goal at MedMatch is to empower primary care physicians with the tools to manage their front office referral process and to stay connected with their specialists, while also facilitating the specialist’s ability to respond effectively to the PCP and their patients’ needs.
The MedMatch Network of pre-screened physicians ensures that the patient is successfully matched to a physician in less time than it takes to enter information in the search criteria on the MedMatch dashboard. For example, with current processes, Doctor A is too busy to see Doctor B’s patient, but Doctor C is one block away and can see Doctor A’s patient. Since neither knows the other exists, the referral never gets made. MedMatch closes this gap. Our cloud-based technology circumvents the use of traditional referral channels such as word-of-mouth, phone, fax, and email which can create more work for the front office and are prone to referral leakage.
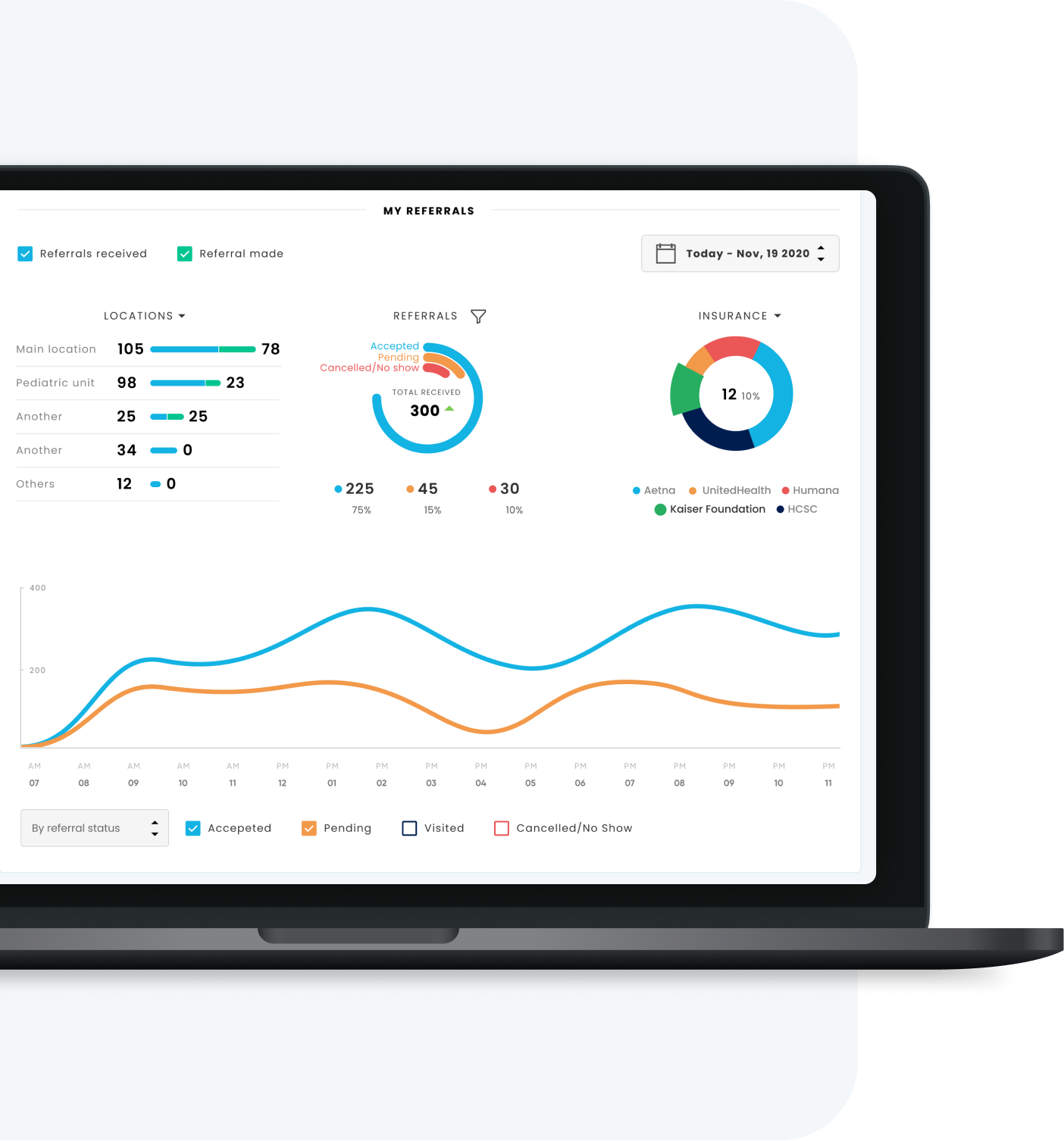
We designed the MedMatch platform to efficiently handle and organize incoming referrals and virtual scheduling. The solution presents referral status and actionable insights for the front desk, thereby saving time. Similarly, outgoing referrals are paperless — no faxes or paper trail means less risk of referral loss. The tracking of outgoing referrals creates a feedback loop to ensure that every referral is accounted for, and the referring physician is informed on the status of each.
The MedMatch platform provides additional communication channels, including SMS texts and emails, which is used to remind patients of their appointment and reduce the rate of “no-shows.” Many EMR platforms provide tools to keep track of “no-shows” so that the office can reschedule these patients. However, it is far better to prevent “no-shows” in the first place to ensure patients get timely care and the doctor’s time is better utilized. Insurance pre-authorization is easily automated, ensuring that the appropriate approval is obtained well before the patient’s appointment.
MedMatch is not only a referral platform; it is also a network of physicians who share a commitment to improving patient care. MedMatch is an interactive online platform where doctors can create their own networks of trusted physicians. Empowering physicians with a network help them safeguard communication, portability of medical records, and continuity of care. The MedMatch Network is a stage for focusing on patient care through referral management. It provides the physician with the tools to stay involved in the patient’s referral journey and ensure a successful and quality referral.
Conclusion
I am passionate about improving healthcare and how technology can help, which lead me to create the MedMatch platform. While we cannot fix all the shortcomings of our excellent healthcare system overnight, we can begin to resolve some of its challenges with the strategic use of technology. Our innovative patient referral management solution is leading the charge in the adoption of medical technology that is highly accessible, secure, easy to use, and affordable. We believe MedMatch will lift some of the barriers to efficient healthcare delivery.