Is Interoperability Another Step Closer to the Patient’s Bedside
A 56-year man is rushed to the hospital after several hours of being stranded in the wilderness; He is delirious and incoherent. An 82-year-old woman is visited by a family member who finds her unconscious in her home alone. A 58-year-old gentleman with Crohn’s disease visits his new primary care physician in a city he just moved to a few weeks ago.
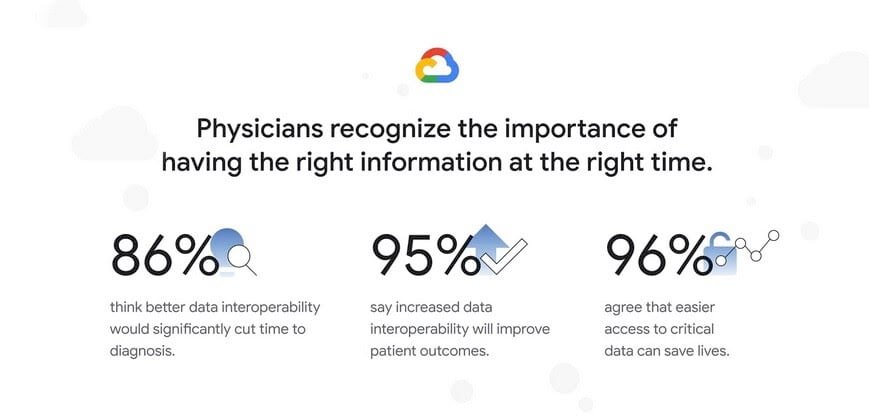
What is the one thing that will make a difference in the diagnosis, management, and long-term outcome of these three patients? You guessed it – timely access to their comprehensive electronic health information, including pre-existing conditions, current medications, and past treatments.
Unfortunately, this type of access to patient information is not readily available at most triage stations in our medical system. Interoperability(1) is not only a buzzword, but it is in fact the connectivity and interface between electronic health record (EHR) systems that can make this magic happen. Here is what the government is doing about it.
Starting with the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009, the U.S. Department of Health and Human Services (HHS) has been nudging the medical community to not only adopt certified EHR systems but also to create a framework that would allow unfettered sharing of health information with patients and their providers, literally at the bedside. The vision of a nationwide health information network storing up-to-date patient information, accessible cross country at a push of a button, was what lead to the creation of the Office of the National Coordinator for Health Information Technology (ONC), an arm of HHS, in 2004.
The federal government’s position was further memorialized in the 21st Century Cures Act signed into law on December 13, 2016. The Law had many objectives.
Title V of the Cures Act– [Delivery]- and its subsequent sections aimed to:
- Assist doctors and hospitals in improving quality of care for patients
- Promote Interoperability
- Prevent Information blocking
- Leverage electronic health records to improve patient care
- Empower patients and improving patient access to their electronic records
The ONC and Centers for Medicare and Medicaid Services (CMS), both part of HHS, has been administering the Cures Act.
The ONC made history on January 18, 2022, with the publication of the first versions of the Trusted Exchange Framework Common Agreement (TEFCA) and its accompanying Technical Framework (2). This milestone marks the beginning of a new chapter in the regulated exchange of electronic health information among health information networks and providers belonging to them. The Common Agreement and its Technical Framework will seek to: 1) Establish a consensus policy and guideline for nationwide interoperability, 2) provide standards for connectivity amongst organizations to securely exchange patient information, and 3) protect and unblock patient access to their health care information.
Together, these objectives are aimed to improve patient care, enhance the welfare of populations, and generate health care value.
Many health providers are connected to electronic health information exchanges (HIE) or networks (HIN). HINs are sprouting across the country supporting communities with a wide range of services. The lack of universal guidelines on patient information exchanges is a common source of friction across networks today.
The impact of the TEFCA may not be apparent immediately to end-users including patients and medical providers for a few months or years to come. The federal government stepping in and setting up guidelines to facilitate data-sharing among HINs will ultimately create a trickle-down effect that will facilitate access to vital medical records needed at the bedside.
It is hoped that the Common Agreement will provide easier ways for individuals and organizations to securely connect and access electronic patient information. It includes support for treatment, payment, health care, operations, individual access services, public health, and government benefits determination. The ONC and its Recognized Coordinating Entity (RCE), The Sequoia Project, are to be commended for achieving this milestone and moving interoperability closer to the patient’s bedside.