Promote Better Patient Experiences Through Enhanced Referral Networks

Now that the federal government has ensured that healthcare providers store patient records electronically, the next challenge is to make sure those records follow the patient wherever they end up. Interoperability enables patient information exchange between different systems throughout the patient journey. This all became possible uder the supervision of medical referral management software.
Interoperability may be required at any point in the patient’s journey – from admission through hospital transfers and discharge; when one doctor refers a patient to another doctor, for diagnostic testing, or for outpatient treatment or care.
Most people in the healthcare industry are familiar with the Health Information Portability and Accountability Act (HIPAA) of 1996 protecting the privacy and security of patient medical information.
Through the 21st Century Cures Act of 2016 (the Cures Act) the federal government stepped in again to ensure that patients have access to and control over their electronic records and that these records are accessible by their providers regardless of where they are kept.
Every year, one of every three patients will be the subject of a referral request. With the COVID-19 pandemic, the need for patient information exchange between medical providers has skyrocketed.
Here is a brief overview of the current state of affairs in many doctor offices and what the MedMatch Network is doing to facilitate interoperability and compliance with new government regulations.
Patient Referrals: 20th Century Practice in the 21st Century
Consider the fax machine. Popular since the 1970s, it is now an increasingly antiquated way of exchanging information. Yet in healthcare, patient referrals are sent by fax machine or its “electronic” version, the efax.
Despite its inefficiencies and security risks:
- In the United States every year about 15 billion patient referral requests still travel by fax.
- In Canada, two-thirds of doctors are still using faxes as their main way of communicating with each other.
- Nearly 7 of every 10 medical specialists who receive a referral request from a primary care provider (PCP) receive no patient information before the initial patient visit.
- After a patient referral visit, the Specialist will provide a patient consultation report to the referring PCP, but only a little more than half the time.
In short, the old technologies for communicating patient information, especially during referrals, are not keeping pace with our increasing healthcare demands even if we don’t consider the current COVID-19 pandemic. Too often PCPs and Specialists are not communicating enough during the referral process.
These inefficiencies are more than sources of frustration for patients and physicians alike. They cost providers, patients, and the government millions of dollars annually due to referral leakage, redundancies in care, medical errors, and delays in care.
What Interoperability Means to Patient Referral

Interoperability is the 21st Century answer to the inefficiencies of fax machines, phone calls, letters, and physical record delivery. It may sound like a buzzword, but interoperability will change the patient referral management ways and how medical professionals build high-quality referral networks.
Technically speaking, interoperability refers to “… policies, practices, and technologies that remove barriers in the patient referral process.”
Practically speaking, interoperability is equivalent to a universal translator for software applications. It establishes a conduit through which otherwise incompatible applications can exchange information.
For patients, interoperability means simplicity, which encourages patient use. Whether an application runs on a computer or a smartphone, regardless of operating system, patients and their physicians can access all their electronic health data from a single application portal.
For healthcare providers, software interoperability in the referral process provides several advantages over fax-based or paper-based requests:
- Interoperability enables the timely exchange of data between referring and receiving doctors, often in near real-time. No more waiting for physical copies to arrive later.
- Having immediate access to all the patient’s health data on receiving the request helps the receiving doctor make better, data-informed decisions about the patient before the initial consultation.
- Interoperability can automate referral tracking and set follow-up reminders. It also facilitates direct patient communication between doctors and supports collaborative treatment plans.
All the above promote a patient journey through the referral process, a more efficient office, savings, and increased revenue capture.
What is the Government’s Interest in Interoperability?
The Cures Act is the wellspring of the federal government’s involvement with interoperability. Under the Cures Act, the Centers for Medicare and Medicaid Services (CMS) work with the Office of the National Coordinator for Health Information Technology (ONC) to promote patient access and healthcare software application interoperability.
Together the CMS and ONC have adopted Health Level 7® (HL7) version 2.5.1 Fast Healthcare Interoperability Resources® (FHIR) Release 4.0.1 application programming interfaces (API) to exchange electronic health data seamlessly and securely.
What are APIs?
APIs are the keys to building software applications that can communicate with one another regardless of their native operating systems. HL7 FHIR standardized APIs open the door for software developers to create compatible patient referral and referral networking applications for providers. They also make it possible for patients to access their own health information from their computers or their smartphones.
How is the Federal Government Promoting Interoperability?
The ONC and CMS are both involved with implementing the Cures Act by creating rule-based milestones for providers, application developers, health information exchanges, and others to implement new interoperability capabilities. In 2021, CMS is enforcing two new interoperability rules:
- Beginning April 1, 2021, hospitals that access EHRs must share with other providers patient admission, transfer, and discharge data.
- Beginning July 1, 2021, payers must support patient access and provider directory APIs.
On April 5, 2021, the ONC implemented information blocking requirements for providers, developers of healthcare IT applications, and health information exchanges. More interoperability and information blocking rules are scheduled for 2022 and 2023.
How Interoperability Enhances Patient Referrals
In a fax-and-paper world, patient referral processing and obtaining patient health records cause delays in the continuum of care. Slower analysis of patient data, based on the review of physical files or fragmented online data systems, causes more patient delays. These delays lead to patient uncertainty, which can lead to missed consults or other lost treatment opportunities – referral leaks.
Seamless access to one’s own health data is important for patients. What matters as much to them is how doctors use that data to optimize assessments, specialty referrals, and treatment plans.
Interoperability is an effective antidote to referral leaks. It also gives doctors the means to provide patients with faster and more personal service. Interoperability improves referral efficiency and security, reducing file handling errors and keeps a patient’s personal health information safe.
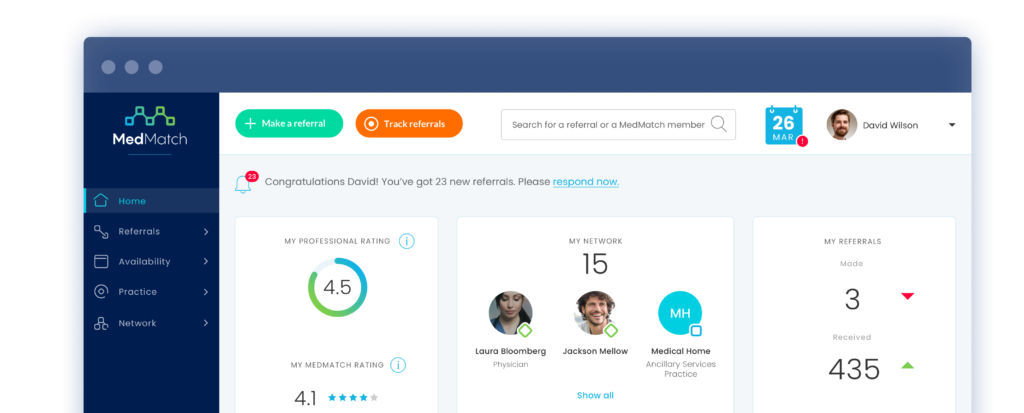
How MedMatch is Implementing Interoperability in Medical Referral Networking
A Secure Way to Communicate and Share Data
The MedMatch platform generates electronic patient referrals. The cloud-based network ensures data security and reduces the processing workload often created by fax or efax referrals.
Improved Referral Efficiency
The quality of a referral is as good as the information that accompanies the patient. The MedMatch Network facilitates patient information exchange with secure, server-less storage in the cloud and integrates with electronic health records (EHR).
Medical providers can simultaneously receive the patient’s entire history along with the referral. This promotes better pre-consult insights, ensures that the referral is appropriate, and expedites decision-making and treatments.
MedMatch’s implementation of healthcare APIs facilitates access to and delivery of patient information where it’s needed most. API access empowers the patient throughout the referral journey, ensuring full participation by the patient along the way. Industry data shows that when patients are motivated about their care plan, they are more inclined to actively participate in their wellness, leading to better outcomes.
MedMatch has fully embraced HL7-FHIR-compliant electronic patient information exchange. Medmatch’s participation in the national trusted health exchange framework as a Qualified Health Information Network (QHIN) facilitates up-to-date and real-time actionable information for patients and their physicians.
Supporting Creation of Professional Referral Networks
Online connectivity and interoperability provide medical professionals with better opportunities to communicate and coordinate with each other. The MedMatch Network is a referral community of medical professionals. The platform eases many of the hurdles, frustrations, and anxiety involved in:
- Finding a physician that takes the patient’s insurance
- Obtaining authorization for the consultation
- Scheduling the patient
- Transmitting all the necessary records, and
- Making sure the patient is informed and shows up for the appointment
MedMatch uses innovative technology, including machine learning, to optimize physician matching and patient referrals. The MedMatch platform is the first medical network using peer-ratings to boost performance.
Use MedMatch Interoperability to Start Making Better Referrals Today
Even doctors who still use faxes to make referrals recognize the potential for interoperability to benefit their practices and patients. Nine of every ten providers surveyed believe that improved interoperability will reduce diagnosis times and improve patient outcomes by making patient data more accessible, and faster than legacy systems.
MedMatch updates fax-driven EHR referrals into today’s interoperability requirements. If you would like to learn more about how MedMatch supports medical referral interoperability, contact one of our medical referral practice experts. Or if you want to see how simple and affordable it is to get started using the MedMatch Network to benefit your patients and your practice, see our resources page.