How ACOs Benefit from Virtual Referral Networking
There is no doubt that health systems play vital role in people’s life but still some problmes are there that sometimes lead to worst situations. A persistent problem in American healthcare is how to control rising care costs without sacrificing care quality. The best way to do this is to reduce unnecessary hospital admissions. Accountable Care Organizations – we will use the term “ACO” from now on – can make a meaningful contribution in this healthcare cost-control. The key is to have a built-in high-value physician referral network to control referral leakage out of the ACO. There are several network recruitment solutions and referral management solutions that can assist ACOs in achieving this goal. These solutions help healthcare systems build a high-value physician referral network, which can ensure that patients receive the appropriate care at the right time and place. Effective referral management solutions can help reduce out-of-network patient leakage by providing real-time visibility into the referral process. This can help providers identify potential referral leakage and take corrective action before it becomes a problem.
In this newsletter we show how a physician referral-networked ACO can keep patient care costs down by reducing out-of-network patient leakage.
Why Participate in an ACO
Every time a patient is admitted to a hospital or clinic it adds to the costs of providing healthcare. An unnecessary admission, whether initial or a readmission, consumes valuable physician time as well as money. Time that a doctor or specialist could be spending more efficiently with existing patient engagement or by seeing more patients. This is where a hospital referral system can play a critical role in managing patient care and reducing unnecessary hospital admissions by enabling better communication and coordination among healthcare providers.
The drain on healthcare personnel and budget resources is serious. Presently about four of every ten patient trips to the emergency department, and one in six inpatient hospitalizations, may be preventable. Hospitals typically see 20 percent of their elderly patients readmitted less than 30 days after discharging them. The costs to Medicare of these readmissions, many of which are unnecessary, is about $17 billion annually.
The more uncoordinated a patient’s healthcare journey is, the more likely it will include unnecessary facility admissions. ACOs exist to empower healthcare providers to reduce unnecessary admissions by coordinating their care services. The objective of this coordination is improving clinical outcomes for their patients while reducing care costs.
What Kinds of ACOs Exist

An ACO may be owned by a single physician group or multiple groups, or by one hospital or multiple hospitals. It may provide healthcare directly to patients or specialize in outpatient services for patient satisfaction. ACOs of all types number around 1,100 in 2021. They take several forms, depending on which of two categories you use: public or commercial.
Public ACOs
The Centers for Medicare and Medicaid Services (CMS) defines a “public” ACO as one that relies on Medicare and Medicaid contracts. These include the Medicare Shared Savings Program (MSSP), the Next Generation model, the End-Stage Renal Disease model, and Pioneer and Advance Payment ACOs.
Commercial ACOs
ACOs not exclusively based on public contracts are commercial ACOs. These ACOs use commercial payer contracts, although many also have Medicare and Medicaid ACO contracts. Independent physician groups, and group alliances, multi-specialty group practices, physician-hospital organizations, virtual physician organizations, expanded physician groups, independent hospitals, and hospital alliances are all examples of commercial ACOs.
Why Network with an ACO
Changes to public ACO programs have slowed the growth of public ACOs since 2019, with exits comprising a quarter of all public ACO contracts. Currently public ACO exits exceed the formation of new ACOs. For example, the number of ACOs in the Medicare Shared Savings Program has decreased from more than 560 in 2018 to fewer than 500 today.
Despite the stagnation of public ACOs, the incentive of an ACO remains improved profitability through shared cost savings. Commercial ACOs have more flexibility than public ACOs do when it comes to how they organize and operate. This is especially so with physician group ACOs, which are the most common form of ACO at about 45 percent of all ACOs.
So why should you consider an ACO in your professional referral networking? Because an ACO remains an effective way to control costs and to better serve your patients. This particularly true for physician-led ACOs consisting of primary health care physicians, physician groups, and medical specialists. who can benefit from utilizing speciality healthcare referrals to efficiently refer patients to the appropriate specialists and subspecialists for their specific healthcare needs, potentially leading to improved patient outcomes and shared cost savings.
Physician Networks are Key to ACO Success

Primary care physicians are at the center of healthcare provider coordination. This is true even outside of an ACO. Even though they are responsible for less than 10 percent of all healthcare spending, through their patient referrals doctors influence the efficiency of downstream patient care spending, whether on additional diagnostic tests, specialist treatment, post-acute, and home care, or other services.
In an ACO environment, the ability of doctors to as much as possible keep patient referrals within the ACO is crucial to achieving cost savings. Despite this knowledge, most ACOs are still not doing enough to coordinate care between primary care physicians and specialists within the organization. This leads to costly patient referral leaks.
How costly? Patient leakage, like a patient’s use of services outside of an ACO, causes at least half of healthcare organizations to lose at least 10 percent of their revenues. Of every five such organizations, one loses more than 20 percent of patient revenue because of out-of-network leakage. And one in four does not know much it loses because it has no way to monitor patient leaks.
An ACO-Friendly Referral Network Can Reduce Patient Leaks
It is easy to sympathize with ACO doctors and specialists who struggle with referral coordination and patient leaks. How to stay on top of all the details, like who is in the ACO, or where they are? What kind of insurance they accept? How they make or accept referrals – are they still using fax machines and sending physical patient records?
What transforms an ACO from a collection of individual providers into a cost-saving team is the ability to coordinate care among members and as much as possible to reduce patient leaks by keeping referrals within the network. This does not have to be hard to do.
The MedMatch Network is specifically designed to simplify the process of creating and managing an ACO for doctors, specialists, and their staff. It supports the specific goals of the ACO and promotes collaboration with other physicians, virtual physician groups, and medical specialists, regardless of their location. ACOs can greatly benefit from a two way referral system where primary care physicians and specialists work together to ensure patients receive appropriate care at the right time and place. Private medical practitioners can also benefit from such systems by building a strong network of physicians to ensure their patients receive appropriate care. Effective referral management solutions can assist private medical practitioners in building such a network by providing real-time visibility into the referral process.
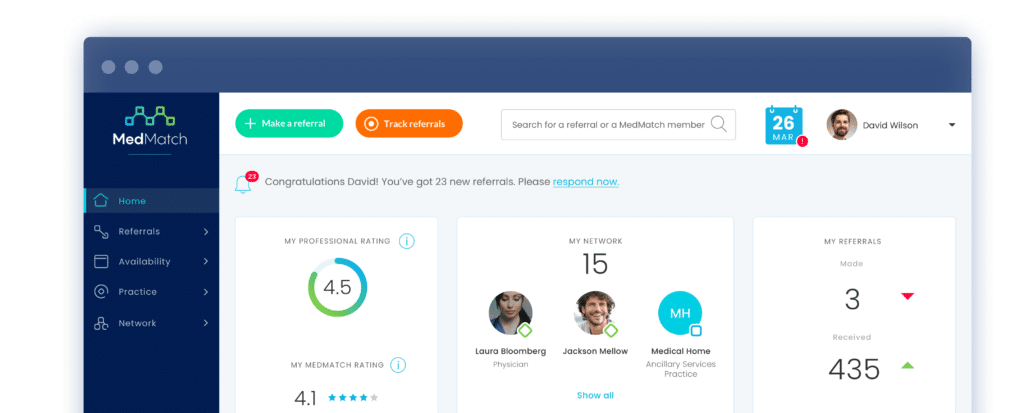
Our MedMatch Network offers a solution for tracking patient referrals and optimizing the referral process. Our patient referral tracking software enables you to manage referrals, exchange patient records and clinical information with referral partners, and improve the coordination of patient care.
With our patient referral tracking process, you can receive actionable referral insights to maximize in-network referrals and improve quality health care services. Our referral tracking software facilitates two-way communications with referral specialists and helps optimize your patients’ healthcare journeys to minimize readmission risks.
If you’re interested in joining our virtual medical referral network and management platform, please contact us to learn more. And if you qualify for our limited-time Charter Member Program, you can receive a free membership in the MedMatch Network.